Table of Contents
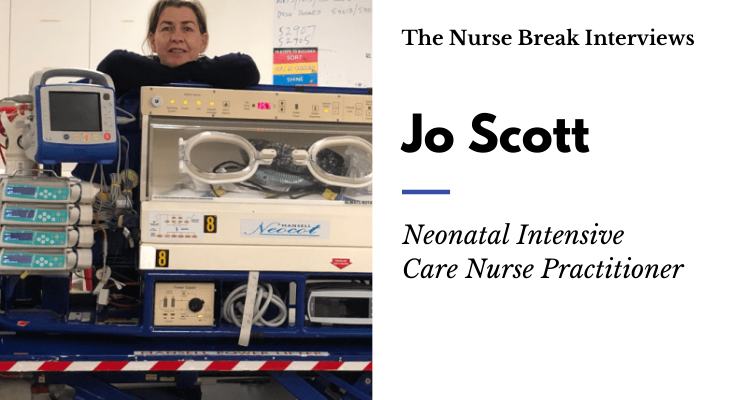
Meet Jo Scott!
Thank you for the opportunity to shine a light on the role of the Neonatal Nurse Practitioner (NNP). I am one of two NNPs working on the Paediatric Infant Perinatal Retrieval (PIPER) at the Royal Children’s Hospital (RCH) in Melbourne. I want to start by saying how much I love my job and the talented team of nurses, doctors and patient transporters I work with on a daily basis.
When I reflect on my career it makes me feel quite old! I started my career in Wellington, New Zealand as Diploma prepared Registered Nurse (RN). I completed my Neonatal Intensive Care Unit (NICU) certification while working at the Wellington Women’s Hospital. Like a lot of other fun-loving Kiwi nurses, I felt the need to spread my wings and work overseas. I started my travels in Honolulu, Hawaii where I worked on my nursing and canoe paddling skills – I accomplished one of my biggest non-nursing achievements when I competed in the international Molokai channel race with an amazing team of women.
I moved from Hawaii to Spokane, Washington State where I continued to work on my NICU nursing skills while raising a young family. It was when my family and I relocated to Charlottesville, Virginia that I was inspired by a strong team of NNPs who encouraged me to pursue the Nurse Practitioner career pathway. While working on the University of Virginia NICU transport team I earned a Master of Science degree as a Family Nurse Practitioner (FNP) and subsequently achieved a Doctorate of Nursing Practice (DNP) and NNP post-graduate certification. Before moving to Australia in 2014 I was working at the Children’s Hospital of the Kings Daughters Hospital in a 72 bed NICU on a team of 20 NNPs.
I joined the RCH NICU team in 2014 when I move to Australia to be closer to family, then joined the PIPER team in 2017.
What is an Nurse Practitioner?
A Nurse Practitioner (NP) is an RN with the experience and expertise to diagnose and treat people of all ages with a variety of acute or chronic health conditions. NP’s have completed additional university study at Master’s degree level and are the most senior clinical nurses in our health care system. The tile “Nurse Practitioner” can only be used by a person who has been endorsed by the Nursing and Midwifery Board of Australia (Australian College of Nurse Practitioners).
What is a Neonatal Intensive Care Unit (NICU) – Neonatal Nurse Practitioner (NNP)?
NNPs originated in the USA in the late 1960s in response to a change in medical training which reduced trainee time in specialist areas, while at the same time there was an increased demand for neonatal care with advances in specialist care and increased survival of premature infants.
An NNP is a highly-skilled, experienced neonatal nurse who delivers direct patient care and incorporates elements of research, education, leadership and incorporated within clinical practice. Like all health care professionals, NNPs have a “scope of practice” to adhere to, allowing them to prescribe medications, order and interpret diagnostic tests, and facilitating communication amongst the multidisciplinary team and NICU families.
Approximately 60 NNPs are working in Australia, a mixture of both endorsed and candidate level NNPs which is an exciting advancement. When I first arrived in Australia 7 years ago, there were only 34.
What does a typical day look like for you?
A retrieval shift is very unpredictable and that is what I like about my job. I am on call for 2 hours before my shift starts, so my day /night often starts prematurely. A shift starts with equipment checks, we do this as a team and if the previous shift has been busy, we may start the shift by cleaning up after our fellow teammates.
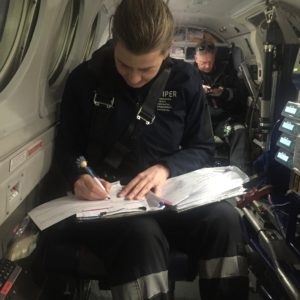
Our retrievals are initiated by a phone call from a referral hospital to our coordination centre which is staffed by Retrieval RNs – the PIPER consultant and retrieval team are paged into the call. When the decision is made to retrieve the infant quick decisions need to be made to determine the mode of transport and team makeup, these decisions are based on the baby’s acuity, location and the weather.
There is no “typical day,” every day is different. Depending on distances travelled and patient acuity you can have up to 4 transports in a 12-hour shift, you can travel by ambulance, fixed-wing aircraft or helicopter. The nature of this job can easily force you into overtime, you may find yourself kilometres from home at the end of your shift, the fog may have set in preventing you from flying home leaving you with a 3-hour drive home with a critically ill baby on board on a bumpy country road. It never pays to make plans for after work – just in case!
What are the main types of patients you see in your current position?
I work on the Neonatal arm of the retrieval team together with a retrieval Neonatal Intensive Care Unit RN we transport neonates up to 8 weeks corrected gestational age with varying degrees of acuity from extremely premature infants to acutely ill asphyxiated term infants.
What is your role in their care and what is the scope of practice of a Neonatal Intensive Care Unit / Neonatal Nurse Practitioner?
The team make up is Fellow or NNP, retrieval RN, and Patient Transport driver (if we travel by road). We are a “team” I do not a make a unilateral decision despite being the team lead, the RN and I work closely together, and I collaborate with the PIPER consultant by phone to discuss the plan of care. Before leaving the referral hospital the nurse and I discuss and prepare for any emergencies that could occur en route. The goal is always to anticipate and be prepared to ensure safe and efficient transport for the best possible patient outcomes.
During transport, the NNP is responsible for performing the advanced clinical skills such as intubation, central and peripheral line placement, chest drain insertion etc.
In line with my scope of practice, my role allows me to diagnose, prescribe, interpret and plan an evidence-based plan of care in conjunction and collaboration with PIPER consultant.
The scope of practice is determined by the nature of the speciality in accordance with the Nursing and Midwifery Board of Australia (NMBA) standards and guidelines; diagnose and treat a wide range of health conditions, design and implement therapeutic regimens, initiate referrals to other health care professionals, order and interpret pathology and radiology tests, prescribe medications.
What are the most rewarding and difficult aspects of your area of work?
It is difficult separating a baby from its family, especially if the baby is critically ill and there is a chance the baby may die before the family can see the infant again. There are so many rewarding aspects of the job including working closely with an extraordinary team, retrieving very sick babies and upon follow up find the baby is progressing well – Good outcomes from the bad situation are “the best”!
What is one thing you wish you would have known before you started your career in this field?
I wish I had known how much I would have loved it and I would have started sooner!!
What is one myth or common misconceptions that you want to debunk about your area.
I speak for myself when I say that NPs do not think they are doctors and do not want to be doctors. I am proud of my Nursing education and bedside experience, but I do embrace the opportunity to bridge the gap between nursing and medical teams.
What advice would you have for other health professionals in dealing with acutely unwell and dying children?
Everyone grieves in their own way – and it is important to give yourself permission to grieve. Don’t be afraid to cry! Find someone you can talk to and if you are having trouble sleeping or emotionally letting go of the death it is important to seek help. It is very easy to “beat yourself up” after the death of a patient in your care.
How do you deal with grief and death?
This is such a hard part of the job, I have only had a couple of deaths on transport, but some of the babies I have transported have died during their NICU stay. As a team we debrief, and the PIPER consultants are very good at checking in after a challenging transport. When at home I go for a long walk or swim laps and take the time to reflect on the transport, I have a good cry and talk with my partner, he doesn’t understand the medical stuff, but he knows had to listen and to gives tight hugs.
How do you destress after a shift and self-care?
Exercise is really important to me, going to the gym or swimming laps helps me relax and gives me time to reflect, especially if I have had challenging transport. Chatting on the phone with my bestie is also a huge part of my self-care routine.
What are some things others can do to better prepare themselves to pursue a career as a Nurse Practitioner?
Find the area of nursing you are passionate about, immerse yourself in that speciality until you are an expert. Take advantage of leadership and education opportunities. Find a mentor who can support you on the educational pathway to becoming an NP.
What pathway would you like to see the future of your profession take over the next 10 years?
Keep the momentum going – promote the education of future NP’s and educate the general public about Nurse Practitioners. I believe that AHPRA should endorse NP’s based on their speciality. We are presently endorsed as NPs with no speciality attached to our titles.
What are some great resources that have helped you along the way?
The resources I use on transport are the RCH practice guidelines, they are easy to access online. Last December I was fortunate to attend a Parliamentary breakfast in Canberra where the Australian College of Nurses (ACN) presented a White Paper; “A new horizon for health service: optimizing advanced practice nursing” which was endorsed by the Minister of Health. This paper promises to optimize Australia’s underutilized senior nursing workforce to bridge a service gap in healthcare for poorly served, underserviced and marginalized populations.
Who are the 3 people who have been most influential to you and why?
- My best friends’ mom (Darlene) – she is smart, kind and the most non-judgemental person I know. Darlene encouraged me to pursue an NNP career.
- The group of NNPs I first worked with at the University of Virginia Hospital – they were exemplary role models.
- My dad, he was one of the hardest working people I know. He started his career as an apprentice plumber and worked his way up to the CEO of the company – a solid role model!
How can we work better with other health professionals in the multi-disciplinary environment?
Nurse Practitioners typically have a good working relationship with the multi-disciplinary team. The relationship could be enhanced with an increased Nurse Practitioner presence in the workforce so they can be utilized to their full potential.
How much non-clinical time do you have?
Four hours a fortnight, the occasional supernumerary day and downtime between retrievals.
What are your nonclinical portfolios?
I write the NNP/Fellow roster, which is a six-month roster, I also pick other projects along the way.
What’s your governance structure?
I report to the PIPER medical director and the director of clinical operations (nursing). I write a monthly report outlining all of my transports, professional development and educational opportunities accessed during the month.
What areas of research are you interested/involved in?
I am presently working on a Bilious Vomit research project with an interested retrieval nurse.
What ongoing professional development do you do to maintain your skills?
I attend medical education opportunities such as simulation labs, case reviews, monthly skills labs, operating theatre for airway skills and NICU monthly education opportunities. I also maintain my USA NNP national certification by attending conferences and taking advantage of online learning opportunities.
Can you think of a really funny situation you’ve had while working?
So many situations come to mind, but a recent one:
I got called into work early and we flew to the country Victoria to pick up a premature baby. With the dad and referral team at the baby’s bedside I took off my sweatshirt to perform a procedure and my shirt was noticeably inside else – I had got dressed in the dark. Everyone thought it was funny and the mood in the room was lightened.
Can you share some night shift tips?
Night shift it so much easier now that my children have grown up and left home. It used to be so challenging trying to fit sleep into my children’s routines. I miss my kids, but I am getting more sleep.
What would you do if you weren’t in your current career?
I would be running a beachside bar in a tropical location.
What’s in your lunch box!
Stay hydrated – I take 2 bottles of sparkling water with ice and lemon to work every shift and I make sure I drink both. I always take a full lunch box to work – retrieval is very unpredictable, so it is important to be prepared and my favourite snack is Vita Wheat crackers with cheese and tomato slices (don’t forget the salt and pepper).
What is one piece of advice for students you would give who are worried about starting a graduate year?
Just do it! Time will pass whether you are in school or not – so you may as well just do it! Learn from your mistakes and don’t be afraid to ask questions.
For more Paediatric content check it out here
Are you an Aussie healthcare professional who would like to write about your area of speciality or other nursing/health related content then please email Jackson at thenursebreak@gmail.com to discuss further or check out the Write for TNB Info Page.









You must be logged in to post a comment.